Pathophysiology
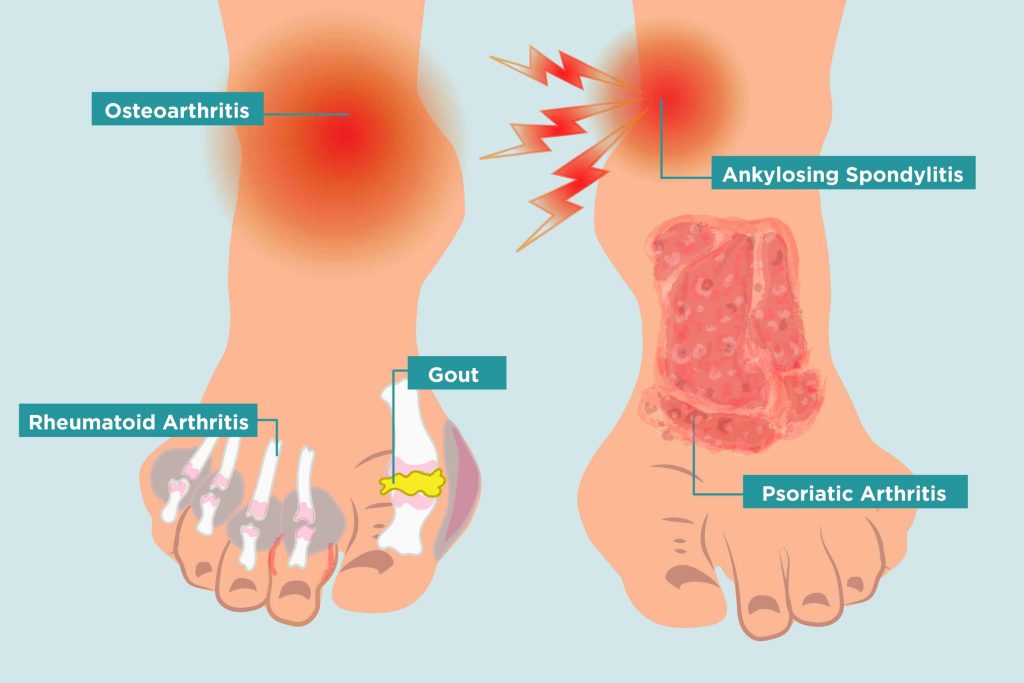
Osteoarthritis is characterized by a degenerative cascade of progressive cartilage loss which leads to bone damage. Characteristic findings include subchondral cysts, osteophytes, and subchondral plate thickening. Interleukin-6, monokines, interferon-induced protein-10, and macrophage chemotactic protein induce proteolytic enzymes such as matrix metalloproteinases, serine proteases, and cysteine proteinases and result in the degradation of joint collage. [16] Calcification of the surrounding articular cartilage reduces the thickness of and eventually destroys the cartilaginous matrix. Old age also is associated with a decrement in chondrocyte function, enhancing susceptibility to osteoarthritic degeneration.
Symptoms of rheumatoid arthritis are typically more severe than those of osteoarthritis. Rheumatoid arthritis is a systemic and chronic inflammatory state caused by an autoimmune response to an environmental trigger. The degradation of cartilage and, eventually, bone is preceded by endothelial cell activation and synovial cell hyperplasia. The pathology occurs following the aberrant production of inflammatory mediators (such as tumor necrosis alpha, interleukins 1, 6 and 8 and others following exposure to an antigenic pathogen). [17]

The monosodium urate salts of gout precipitate as needle-shaped crystals. This crystallization is more likely to occur in cooler body parts and with acidic conditions. Destabilization of these deposited intraarticular uric acid crystals leads to IL-1 mediated inflammatory response leading to the typical acute gouty arthritis flare. The process is different in pseudogout where the inorganic pyrophosphate from chondrocytes combines with calcium to form calcium pyrophosphate dihydrate. This crystal is deposited in joint spaces that have a predilection to osteoarthritic changes. Pseudogout crystal damage includes the fragmentation of bone and cartilage and the formation of osteophytes and subchondral cysts. Metabolic disorders such as hemochromatosis, hyperparathyroidism, or hypomagnesemia increase the likelihood of calcium pyrophosphate deposition. [18]
Septic arthritis is typically an inflammatory response to a monobacterial infection. Bacterial entry into the synovial fluid triggers a release of cytokines, chemokines, and proteases that degrade cartilage and trigger hyperplasia of the synovial membrane. Toxins produced by bacteria play an additional destructive role within the joint space itself. In adults, Staphylococcus aureus is the most common pathogen (with streptococci strains also being common). [19] Infection by gram-negative bacteria is more commonly seen as a result of trauma, intravenous drug use, immunosuppression, or in the elderly or very young.
History and Physical
History and physical examination plays a crucial role in the evaluation of arthritis and determining the type of arthritis, and differentiating symptoms from non-articular etiologies. The 1st step in the physical examination of a patient with musculoskeletal complaints should be determining and confirming if the pain is articular or not. Non-articular pain can be seen secondary to several pathologies including fibromyalgia, where patients have tenderness in articular as well as extra-articular areas, but no effusion, swelling, warmth or erythema localized to the joints. Tendinitis can also cause periarticular pain, a physical exam in these cases usually reveals tenderness along the tendon course or insertion without any focal tenderness or loss of range of motion of the joint.
Usual symptoms of arthritis are pain, swelling, loss of function, stiffness, deformity, weakness, and instability. They may also be accompanied by fatigue, sleep disturbance, emotional liability and symptoms of the underlying systemic illness. Pain from arthritis is usually worse by activities and at the end of the day. Inflammatory arthritis will also cause pain in the morning and at rest that may initially improve with activity, but subsequently gets worse with prolonged use and activity. Patients with fibromyalgia and myofascial pain syndrome usually complain of a diffuse all over pain. Neuropathic pain can be accompanied by paraesthesias in the nerve distribution. Morning stiffness lasting more than 45 minutes is typically associated with inflammatory arthritis, [20] but this is non-specific as patients with osteoarthritis or non-articular syndromes such as fibromyalgia can also have prolonged morning stiffness.